Role of Hyperbaric Oxygen Therapy (HBOT) in Osteomyelitis
Osteomyelitis
What is Osteomyelitis?
Osteomyelitis is an infection-related inflammation or swelling of the bone tissues. Bone infections can affect both children and adults and can happen for a variety of causes. A systemic bacterial infection that spreads to the bones, often known as sepsis or bacteremia, can result in osteomyelitis. This form typically affects a child’s long bones, such as the femur (thighbone) or humerus, and is most prevalent in infants and young children (upper arm bone). Adult cases of osteomyelitis frequently involve the vertebral bones along the spinal column. Staphylococcus aureus is typically the cause of the blood infection, while other bacteria or fungi may also be to blame. Osteomyelitis is more prone to occur in those with compromised immune systems. People who have sickle cell disease, HIV, or who are taking immunosuppressive drugs like chemotherapy or steroids fall under this category. Depending on the cause of the infection, osteomyelitis may start suddenly, slowly, and mildly, or it may develop into a chronic condition. Out of every 10,000 people, 2 to 5 will get osteomyelitis. One of the earliest known disorders and its origins have been established to be more than 250 million years old [1].
Types
The following are osteomyelitis subtypes:
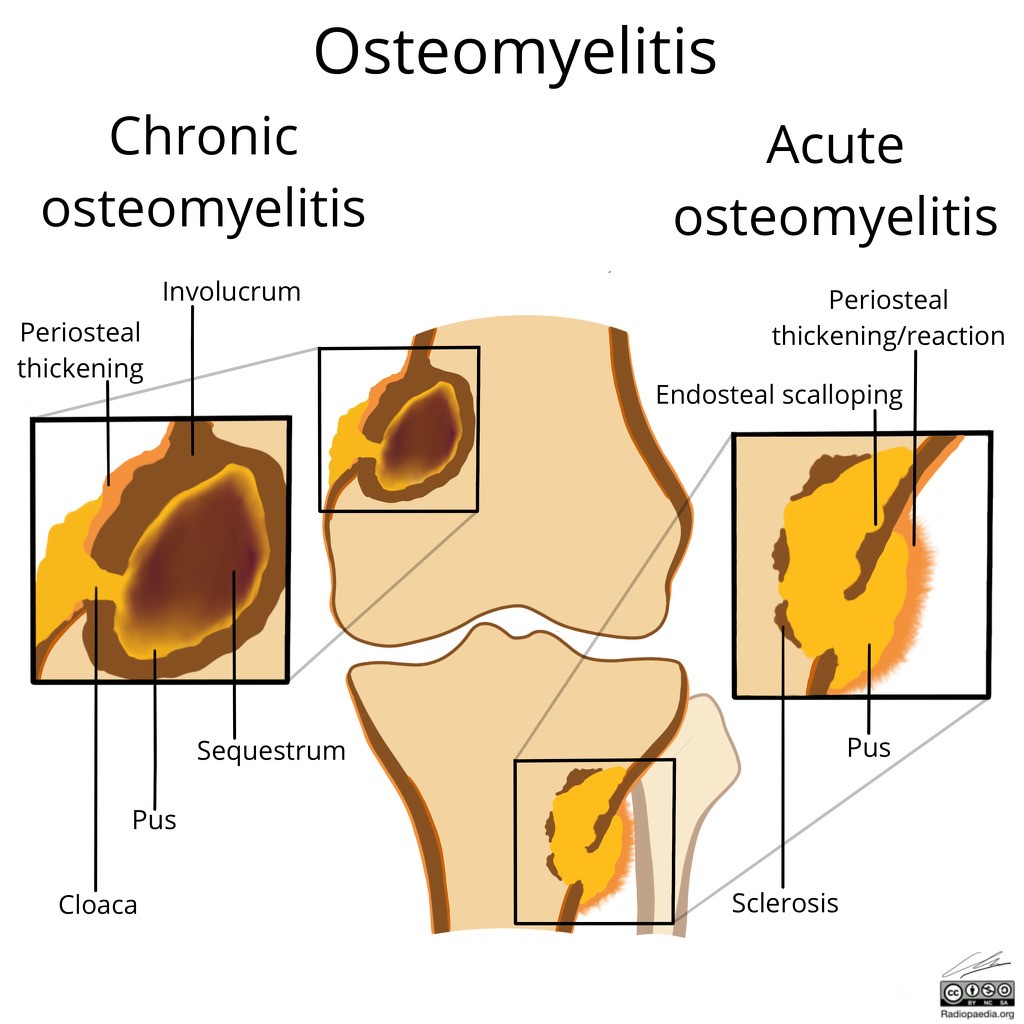
- Acute: The onset of this infection is abrupt. You might have a fever for a few days before experiencing pain in the infected area.
- Chronic: Chronic osteomyelitis is an infection of the bones that is resistant to medical care. It results in persistent leakage and bone pain. Occasionally, persistent osteomyelitis goes undiagnosed.
- Vertebral: The spine is affected by this type. It results in persistent back pain that worsens as you move. It seldom results in a fever. Spinal bone infections are more common in people who reside in nursing homes, abuse intravenous medications, or are receiving dialysis [2].
Causes
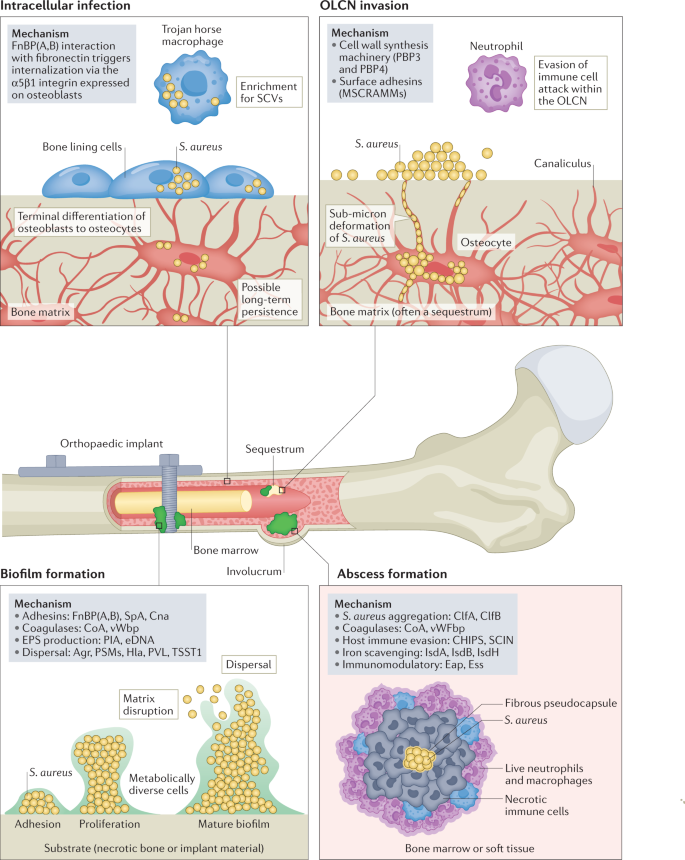
Osteomyelitis develops when germs travel via your blood from adjacent sick tissue or an open lesion and land in bone, where they multiply. Osteomyelitis is frequently caused by infections, or Staphylococcus aureus bacteria. A bone infection can occasionally be brought on by a fungus or other microbe. Staphylococcus aureus is the etiological pathogen in 30% to 60% of human osteomyelitis cases, while staphylococci as a group are responsible for about 75% of cases. Osteomyelitis is an infectious disease that affects the bone and bone marrow. Osteomyelitis typically results from a traumatic or hematogenous cause. Children under the age of 16 are most frequently affected by the hematogenous spread of germs, which causes hematogenous osteomyelitis [3].
The following conditions increase your risk of developing osteomyelitis:
- A hip replacement is an artificial joint
- disorders including sickle cell anaemia or blood infections
- Diabetes, particularly a foot ulcer brought on by diabetes
- bone implants made of metal, like screws
- pressure wounds (bedsores)
- recent bone surgery or bone fracture
- traumatic wound or injury
- inadequate immune system
Symptoms
The infected area may also be red, heated, swollen, and painful to the touch. As further indications of osteomyelitis include:
- Drainage (yellow pus)
- irritability or sluggishness
- Painful and restricted movement.
- decrease in appetite.
- a lower back aches
- vomiting and nausea
- chills
Diagnosis
Your doctor may recommend one or more of the following tests after evaluating your symptoms and conducting a physical examination:
- Complete blood counts (CBCs) in blood tests look for indicators of infection and inflammation. An examination of your blood culture checks for germs.
- Images of your bones, muscles, and tissues are produced by imaging tests like X-rays, MRIs, CT scans, and ultrasounds.
- Bone scan: During an imaging scan, a bone scan employs a little amount of harmless, radioactive material to find infections or fractures.
- Biopsy: A needle biopsy is conducted by your healthcare professional to obtain samples of fluid, tissue, or bone that will be examined for indications of infection.
Treatment
Healing from a bone infection might take an exceptionally long time. If you begin therapy within three to five days after first seeing symptoms, the infection can go away more quickly.
Treatments include:
- Antibiotics: Antibiotics eliminate microorganisms that cause infections. Antibiotics may be required for four to eight weeks, beginning with intravenous (IV) antibiotics administered in the hospital for one or two weeks. After that, you will take drugs orally for a few weeks. Antibiotics may be needed for months to treat chronic illnesses.
- Antifungals: You may need to take oral antifungal drugs for months to treat fungal infections.
- Your healthcare professional will use a tiny needle to aspirate the pus and liquid from the abscess.
- Nonsteroidal anti-inflammatory medications (NSAIDs) are used to treat inflammation and pain.
- In some cases, surgery is required to treat bone infections. After surgery, antibiotics will be required. the following surgical options:
- Bone surgery: The infected, dead tissue and bone are surgically removed (debrided) by your healthcare practitioner. Bone abnormalities could develop because of this surgery.
- Those who have vertebral osteomyelitis may require spine surgery. By doing this operation, you can prevent vertebrae from collapsing and harming your spinal cord, nerves, and other nervous system components [4].
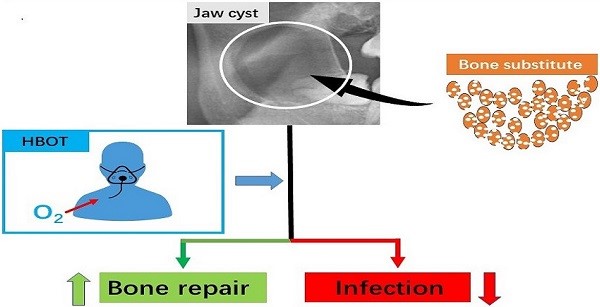
Hyperbaric Oxygen as Effective Medicine for Osteomyelitis
By administering pure oxygen under high pressure, hyperbaric oxygen treatment (HBOT) increases the amount of oxygen in the blood and tissues (hyperoxia) (about 2-3 atmospheres). One method of treatment involves being exposed to pure oxygen (O2) concentrations at high atmospheric pressures using hyperbaric oxygen therapy (HBOT). According to the Undersea and Hyperbaric Medical Society, this pressure may be greater than or equivalent to 1.4 atmospheres. For all current UHMS-approved uses, patients may only inhale oxygen when restrained in a space with a minimum air pressure of 2 ATA. For hyperbaric medicine to work, there needs to be a pressure environment that is greater than the air pressure at sea level. Hyperbaric oxygen treatment (HBOT) has been shown to rejuvenate bone cells and encourage natural development. Collagen is needed to fill up the spaces between broken bones so they can heal, and HBOT promotes its production. Hyperbaric oxygen may also promote the growth of osteoblasts and osteoclasts, two cell types necessary for breaking down old, dead bone and forming new bone.
Most existing animal data, human case series, and non-randomized prospective trials point to the safety and improved infection resolution rates of adding hyperbaric oxygen (HBO2) therapy to normal surgical and antibiotic management in previously resistant osteomyelitis. HBO2 treatment should therefore be regarded as an American Heart Association (AHA) Class II recommendation in the treatment of refractory osteomyelitis. HBO2 therapy can be categorized as an AHA Class IIb therapy in cases of uncomplicated extremities osteomyelitis or situations where severe patient morbidity or mortality is unlikely to occur. Most of the time, HBO2 therapy that is combined with antibiotics that are targeted to a particular culture and are started quickly after a thorough surgical debridement yields the greatest clinical results. Typically, 2.0-3.0 atmospheres of absolute pressure are used to administer HBO2 therapy daily for 90 to 120 minutes (ATA).
By stimulating both the osteoclasts and the osteoblasts, HBOT can aid in the healing of bone diseases. This promotes the formation of new bone and aids in the resorption of dead bone. Additionally, HBOT promotes the growth of new blood vessels, ensuring a consistent supply of nutrients, including oxygen, for the developing bone. Additionally, this blood artery network supplies infection-fighting white blood cells to the region and aids in supporting osteoclast function. Osteomyelitis is a bacterial infection that typically affects the interior bone marrow as well as the outer layers of the bone. A typical type of bacteria called staphylococci can result in diseases ranging from acne to meningitis. If the acute form of osteomyelitis is not fully cured by treatment, chronic osteomyelitis may develop over time or follow an acute form. Refractory osteomyelitis is a phrase used to describe a bone infection that did not improve with medical intervention or antibiotic treatment. Osteomyelitis generates an oxygen shortage in the tissues, which contributes to its difficulty in treatment. Along with antimicrobial medication and/or surgical intervention, HBOT, which provides forced oxygenation, aids in the treatment of this condition. The immune system is aided by hyperbaric oxygen therapy, which also helps to restore and assist create new bone. HBOT can sometimes draw a precise line that allows the surgeon to assist in the excision of sick or dead bones in both bones and wounds. These infections can occasionally develop after tooth extraction.
HBOT promotes the healing of hypoxic tissue by giving fibroblasts, the cells that form connective tissues, enough oxygen. Osteoclasts, which remove dead bone, require oxygen to operate, and the development of new blood vessels requires intermittent oxygen pressures of 30 to 40 mmHg. HBOT is bacteriostatic (bacteria-stopping). For neutrophils to effectively fight germs, they need a PO2 of 30 to 40 mmHg. HBOT increases the effectiveness of several sulfonamides, quinolones, and aminoglycoside antibiotics. It increases the inflammation that frequently follows surgical treatment for refractory osteomyelitis by preventing polymorphonuclear (PMN) leukocytes (white cells) from sticking to damaged blood vessel linings.
When Moorey et al. (1979) used HBOT to treat 40 cases of chronic osteomyelitis, 89.5% of the patients no longer displayed any osteomyelitis-related clinical symptoms.
For nine patients with jaw osteomyelitis, Jamil et al. (2000) found a significant improvement.
An examination of patients who underwent cardiothoracic surgery and sternotomies between 2002 and 2009 and experienced osteomyelitis and sternal infections. Six of the twelve patients who had debridement and antibiotic therapy were also given supplemental HBO2 therapy. Compression, oxygen breathing, and decompression were the three phases of each 120-minute session. With ambient air, compression and decompression were carried out at a rate of 0.1 ATA per minute. During the oxygen breath phase, all patients used a face mask that was properly fitted and fastened with head straps for 90 minutes of 100% oxygen breathing at 2.5 ATA. By increasing tissue oxygen partial pressure, HBO2 inhibits infection, speeds up the healing of wounds, and has a synergistic impact with some medications. In this study, all patients who received HBO2 therapy as an additional treatment for sternal infection and osteomyelitis related to post-cardiothoracic surgery had successful outcomes.
References
- Matteson EL, Osmon DR. Infections of bursae, joints, and bones. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020: chap 256.
Link: https://mayoclinic.pure.elsevier.com/en/publications/infections-of-bursae-joints-and-bones
- Raukar NP, Zink BJ. Bone and joint infections. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018: chap 128.
Link: https://www.sciencedirect.com/science/article/pii/S0196064406021433
- Mader, Jon T., et al. “Osteomyelitis.” Expert guide to infectious diseases (2002): 585-604.
Link: https://www.cabdirect.org/cabdirect/abstract/20053199929
- Calhoun, Jason H., M. M. Manring, and Mark Shirtliff. “Osteomyelitis of the long bones.” Seminars in plastic surgery. Vol. 23. No. 02. © Thieme Medical Publishers, 2009.
Link: https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0029-1214158
- Hanley, Mary E., Stephen Hendriksen, and Jeffrey S. Cooper. “Hyperbaric treatment of chronic refractory osteomyelitis.” StatPearls [Internet]. StatPearls Publishing, 2022.
Link: https://www.ncbi.nlm.nih.gov/books/NBK430785/
- Savvidou, Olga D., et al. “Effectiveness of hyperbaric oxygen therapy for the management of chronic osteomyelitis: a systematic review of the literature.” Orthopedics 41.4 (2018): 193-199.
Link: https://journals.healio.com/doi/abs/10.3928/01477447-20180628-02
- Jamil, M. U., A. Eckardt, and W. Franko. “Hyperbare Sauerstofftherapie Klinische Anwendung in der Behandlung von Osteomyelitis, Osteoradionekrose und der Wiederherstellungschirurgie des vorbestrahlten Unterkiefers.” Oral and Maxillofacial Surgery 5.4 (2000): 320-323.
Link: https://www.infona.pl/resource/bwmeta1.element.springer-c350c203-d130-3fa7-890f-3d1a90b8272e
- Yu, WK., Chen, YW., Shie, HG. et al. Hyperbaric oxygen therapy as an adjunctive treatment for sternal infection and osteomyelitis after sternotomy and cardiothoracic surgery. J Cardiothorac Surg 6, 141 (2011). https://doi.org/10.1186/1749-8090-6-141.
Link: https://cardiothoracicsurgery.biomedcentral.com/articles/10.1186/1749-8090-6-141#citeas

