Role of Hyperbaric Oxygen Therapy (HBOT) in Liver Diseases
Liver Diseases
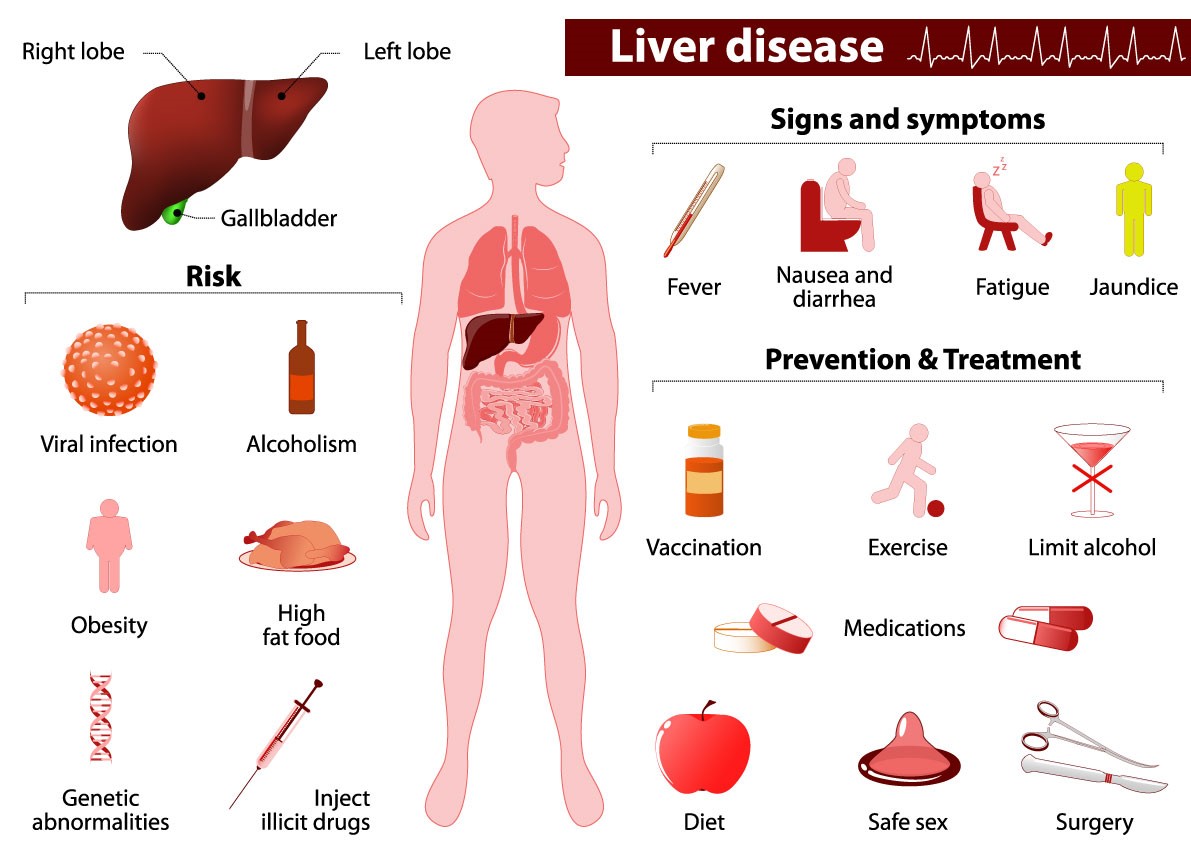
The liver is a crucial organ that carries out numerous metabolic, energy-storing, and waste-filtering functions. It aids in food digestion, energy production, and energy storage needed. Any ailment that affects your liver is referred to as having liver disease. All these disorders have the potential to harm your liver and impair its functionality, however, their causes may vary. Liver disease may run in families (genetic). Viruses, alcohol use, and obesity are just a few examples of the many variables that can harm the liver and result in liver disorders. The next big lifestyle illness after diabetes will be liver disease. Although anybody can get liver disease, many individuals are between the ages of 40 and 60. Liver disease is the tenth most common cause of mortality in India, according to WHO statistics. Some facts about liver diseases are:
- Liver disease may impact every fifth person in India.
- In India, cirrhosis of the liver is diagnosed in close to 10 lakh persons each year.
- In the world, hepatocellular carcinoma (HCC) is the second most frequent cause of cancer-related mortality.
- The 14th leading cause of death worldwide is liver cirrhosis [1].
Types of Liver Diseases
The following are some of the most prevalent kinds of liver diseases:
- Viral infections: Hepatitis A, B, and C are conditions brought on by a viral infection.
- Having immune system issues: Autoimmune liver problems can result from your immune system wrongly attacking your liver. These include autoimmune hepatitis and primary biliary cholangitis.
- Inherited diseases: Some liver issues arise because of a genetic disorder (the one you inherit from your parents). Hemochromatosis and Wilson disease are two examples of inherited liver conditions.
- Cancer: Tumors may form in your liver when abnormal cells proliferate there. These tumours could be malignant or benign (non-cancerous).
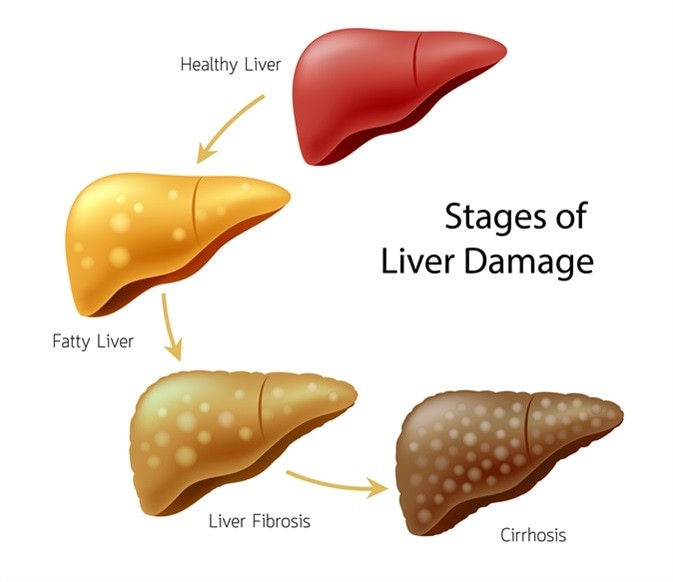
- Consuming excessive amounts of toxins: Abuse of alcohol can lead to alcoholic fatty liver disease. Consuming excessive amounts of fat causes non-alcoholic fatty liver disease (NAFLD). As the prevalence of obesity and diabetes rises, NAFLD is becoming more widespread [2].

Common Symptoms
By the time liver disease, symptoms appear, your liver has already suffered injury and scarring. The term for this is cirrhosis. Some common symptoms are:
- feeling always exhausted and weak
- a decrease in appetite that could cause weight loss
- the decline in sexual desire
- both the skin and eye whites are yellow (jaundice)
- You can also have other symptoms like itching skin or a sickly feeling
Depending on the underlying aetiology, several symptoms of liver disease exist. Additionally, a person with liver illness may not exhibit any symptoms at all. However, according to Hepatitis NSW, a few broad signs may point to serious liver disease of some form.
These consist of:
- Jaundice is characterized by yellowish skin and eyes.
- Bloody, white, or dark stools
- ascites-related enlargement of the stomach, which could make it unpleasant to eat or lie down
- encephalopathy, a condition of the brain that causes significant alterations in mood, sleep, and cognition.
Causes
- Infections
Hepatitis viruses, such as the following, are the most prevalent causes of liver infection:
- Influenza A
- Hepatitis B
- Hepatitis C
- Immune system Abnormalities
Your liver may be impacted by autoimmune diseases, which occur when your immune system assaults particular body organs. Various autoimmune liver conditions include:
- Hepatitis autoimmune
- biliary cholangitis primary
- First-stage sclerosing cholangitis
- Cancer
Examples comprise:
- liver tumours
- Biliary duct cancer
- liver tumour
- Genetics
The buildup of numerous substances in your liver can result in liver disease if you have a faulty gene that you either received from one of your parents or both. genetic hepatic conditions comprise:
- Hemochromatosis
- Wilson’s illness
- a lack of alpha-1 antitrypsin
- Other
The following are additional, typical causes of liver disease:
- long-term alcoholism
- A buildup of fat in the liver (nonalcoholic fatty liver disease)
- certain over-the-counter or prescription drugs
- a few herbal ingredients [3].
Risk factors
You may be more vulnerable to developing the liver disease if you have:
- heavy drinking
- Obesity
- diabetes type 2
- Body art or piercings
- drug injection using shared needles
- Transfusion of blood
- exposure to bodily fluids and blood of others
- Unrestricted sex
- exposure to certain poisons or substances
- an inheritance of liver illness
Diagnosis
These may consist of:
- Liver enzyme levels are measured through blood tests using liver enzymes. The international normalized ratio, a blood-clotting test, is one of the further assessments of liver function (INR). Unusual amounts could be a sign that your liver is not working properly.
- Imaging tests: Your doctor may use an ultrasound, MRI, or CT scan to check your liver for evidence of injury, scarring, or malignancies. The degree of liver fat deposition and scarring can be assessed using the fibro scan, a different specialized form of ultrasound.
- Liver biopsy: A tiny sample of liver tissue is taken during a liver biopsy by your doctor using a fine needle. To search for indicators of liver illness, they examine the tissue.
Treatment
The sort of liver illness you have and how far it has advanced will determine how it is treated. Treatment options include:
Medication for high blood pressure antiviral medications to treat hepatitis steroids to reduce liver inflammation
Antibiotics drugs that address symptoms, like itchy skin vitamins and supplements that improve liver health
Lifestyle modifications: You can manage some types of liver disease with your diet. Alcohol should be avoided, fat and calorie intake should be reduced, and fiber intake should be increased if you have fatty liver disease. Alcohol abstinence can help liver damage caused by alcohol.
Liver transplant: A liver transplant may be the best course of treatment when hepatic disease leads to liver failure. Your liver is replaced by a healthy liver during a transplant [4].
Hyperbaric Oxygen as Effective Medicine for Liver Diseases
By applying pure oxygen at high pressure (about 2-3 atmospheres), hyperbaric oxygen treatment (HBOT) increases the amount of oxygen in the blood and tissues (Hyperoxia). Hyperbaric oxygen therapy (HBOT), a type of treatment, involves being exposed to pure oxygen (O2) concentrations at high atmospheric pressures. According to the Undersea and Hyperbaric Medical Society, this pressure may be greater than or equivalent to 1.4 atmospheres (atm) (UHMS). All existing UHMS-approved indications, however, call for patients to be confined in a chamber with a minimum pressure of 2 ATA and to breathe only with oxygen. A pressure chamber, which can have a flexible or rigid form, and a mechanism to deliver 100% oxygen are required for hyperbaric oxygen therapy. A predetermined plan is followed by trained professionals who keep an eye on the patient and change the timetable as needed.
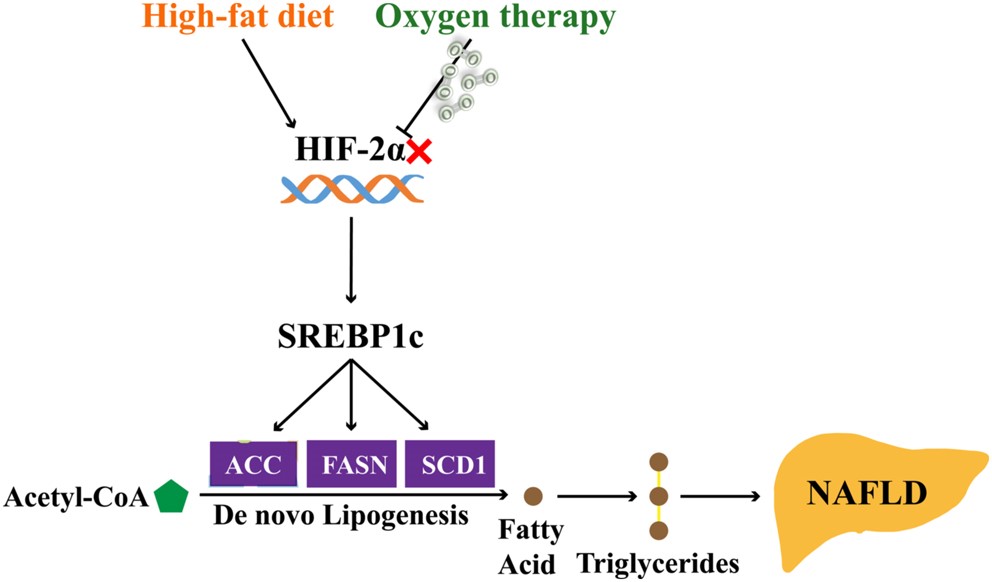
Due to a lack of efficient treatments, non-alcoholic fatty liver disease (NAFLD) is challenging to control. Hepatic steatosis is brought on by increased oxygen use brought on by overeating and decreased oxygen supply to liver cells. Researchers investigated how well HBOT worked to treat hepatic steatosis. In mice fed a high-fat diet (HFD) and primary hepatocytes treated with palmitic acid (PA), the impact of HBOT on hepatic steatosis was examined. Then, the mice or cells from the HBOT group were transferred to the oxygen chamber. One of the holes was used to ventilate the oxygen chamber using a pipe that was attached to 100% oxygen for one minute, after which the oxygen chamber’s door was shut and the other hole was linked to the outside. Based on the measurement from the oxygen meter, the chamber’s oxygen level was kept between 88% and 100%. In HFD mice, HBOT improves glucolipid abnormalities associated with NAFLD, reduces lipid droplets in hepatocytes pre-treated with PA, and safely and effectively alleviates hepatic hypoxia and steatosis. The HBOT-mediated suppression of hepatic HIF-2 expression may be crucial in the management of NAFLD [5].
90 male rats were placed into six groups in a different study. Six HBO sessions totalling 90 minutes each were conducted at 2 atm absolute, spaced six hours apart. As a result, they found that HBOT might be a valuable adjuvant therapeutic approach to increase the effectiveness of sepsis treatment [6].
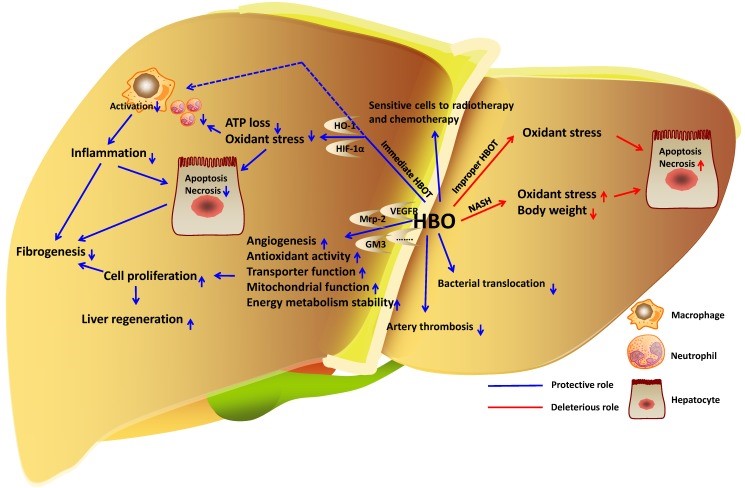
Immediate HBOT in the liver lowers oxidative stress and inflammation to safeguard hepatocytes in liver injury. HBOT also promotes fibrogenesis and hepatocyte proliferation. HBOT prevents bacterial translocation to lessen liver damage brought on by sepsis. Additionally, HBOT is unquestionably a successful treatment for arterial thrombosis. Although the function of HBO in the growth of liver cancer cells is unknown, a combination of HBOT plus radiotherapy or chemotherapy can kill cancer cells. However, inappropriate HBOT causes oxidative stress and hepatotoxicity to worsen.
In therapeutic situations, hyperbaric oxygen treatment (HBOT) has been shown to alleviate liver dysfunction and increase oxygen delivery to ischemic tissues. Rats that had undergone 90% hepatectomy underwent HBOT to see how it affected the regeneration of the remaining liver. Male Wistar rats who were 8 weeks old and had had 90% hepatectomy were separated into two groups: HBOT (2 atm abs., 80% O2, 1 h/day, 3 days) and non-HBOT. When compared to the non-HBOT group, the HBOT group’s liver regeneration rate at 36- and 50-hours following surgery and the percentage of PCNA-positive cells after 8 hours were both significantly higher. At 12 hours, the HBOT group’s leftover livers showed a considerable increase in ATP volume [7].
Noise exposure is linked to several pathological conditions, including liver damage, for which preventative measures are being used. As a non-invasive process, hyperbaric oxygen therapy (HBOT) has a strong therapeutic effect on a variety of liver illnesses. Mice were exposed to broad band noise for 5 days, 3 hours every day (20-20 k Hz, 90-110 dB). Before being exposed to noise, HBOT with a 2.5 atmosphere absolute (ATA) was used. Hematoxylin-eosin (HE) staining was used to analyze the morphology of liver tissue. In noise-exposed mice, HBOT decreased the percentage of apoptotic hepatocytes, reducing the amount of superoxide produced. In noise-exposed mice, HBOT reduces liver structural and functional abnormalities by blocking the ASM/Cer pathway [8].
References
- Mann, Robert E., Reginald G. Smart, and Richard Govoni. “The epidemiology of the alcoholic liver disease.” Alcohol research & health 27.3 (2003): 209.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668879/
- Bosch, F. Xavier, et al. “Primary liver cancer: worldwide incidence and trends.” Gastroenterology 127.5 (2004): S5-S16.
Link: https://www.sciencedirect.com/science/article/abs/pii/S0016508504015902
- Ahmed A, Wong RJ, Harrison SA. Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Clin Gastroenterol Hepatol. 2015;13(12):2062–70.
Link: https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-022-00980-1
- Crabb, David W., et al. “Diagnosis and treatment of alcohol‐associated liver diseases: 2019 practice guidance from the American Association for the Study of Liver Diseases.” (2020).
- Yu, L., Wang, H., Han, X., Liu, H., Zhu, D., Feng, W., … & Bi, Y. (2020). Oxygen therapy alleviates hepatic steatosis by inhibiting hypoxia-inducible factor-2α. Journal of Endocrinology, 246(1), 57-67.
Link: https://joe.bioscientifica.com/view/journals/joe/246/1/JOE-19-0555.xml
- Oter, S., Edremitlioglu, M., Korkmaz, A. et al. Effects of hyperbaric oxygen treatment on liver functions, oxidative status, and histology in septic rats. Intensive Care Med 31, 1262–1268 (2005). https://doi.org/10.1007/s00134-005-2701-6.
Link: https://link.springer.com/article/10.1007/s00134-005-2701-6#citeas
- Nagamine, K., et al. “Beneficial effect of hyperbaric oxygen therapy on liver regeneration after 90% hepatectomy in rats.” European surgical research 36.6 (2004): 350-356.
Link: https://www.karger.com/Article/Abstract/81643
- Meng, Xingxing, et al. “Hyperbaric oxygen treatment mitigates liver damage in mice with noise exposure.” Clinical and Experimental Pharmacology and Physiology 47.9 (2020): 1564-1574.
Link: https://onlinelibrary.wiley.com/doi/10.1111/1440-1681.13330

