Role of Hyperbaric Oxygen Therapy in Sensorineural Hearing Loss
Sensory Hearing Loss
Sudden deafness is another name for sudden sensorineural hearing loss (SSHL). It happens when you suddenly lose your hearing, usually only in one ear. It could take place all at once or spread out over several days. The sound eventually becomes faint or muted throughout this time.
Hearing loss of at least 30 dB that occurs over at least three successive audiometric frequencies and lasts for at least three days is known as sudden sensorineural hearing loss (SSNHL). Only 10 to 15 percent of cases have a known aetiology, and the vast majority are classified as idiopathic. Patients frequently experience auditory fullness or obstruction when they initially wake up with symptoms. They might also experience vertigo, nausea, or tinnitus. Since many patients do not seek medical attention, it is challenging to estimate the spontaneous recovery rate, however, it has been estimated to range from 25 to 65 percent [1].
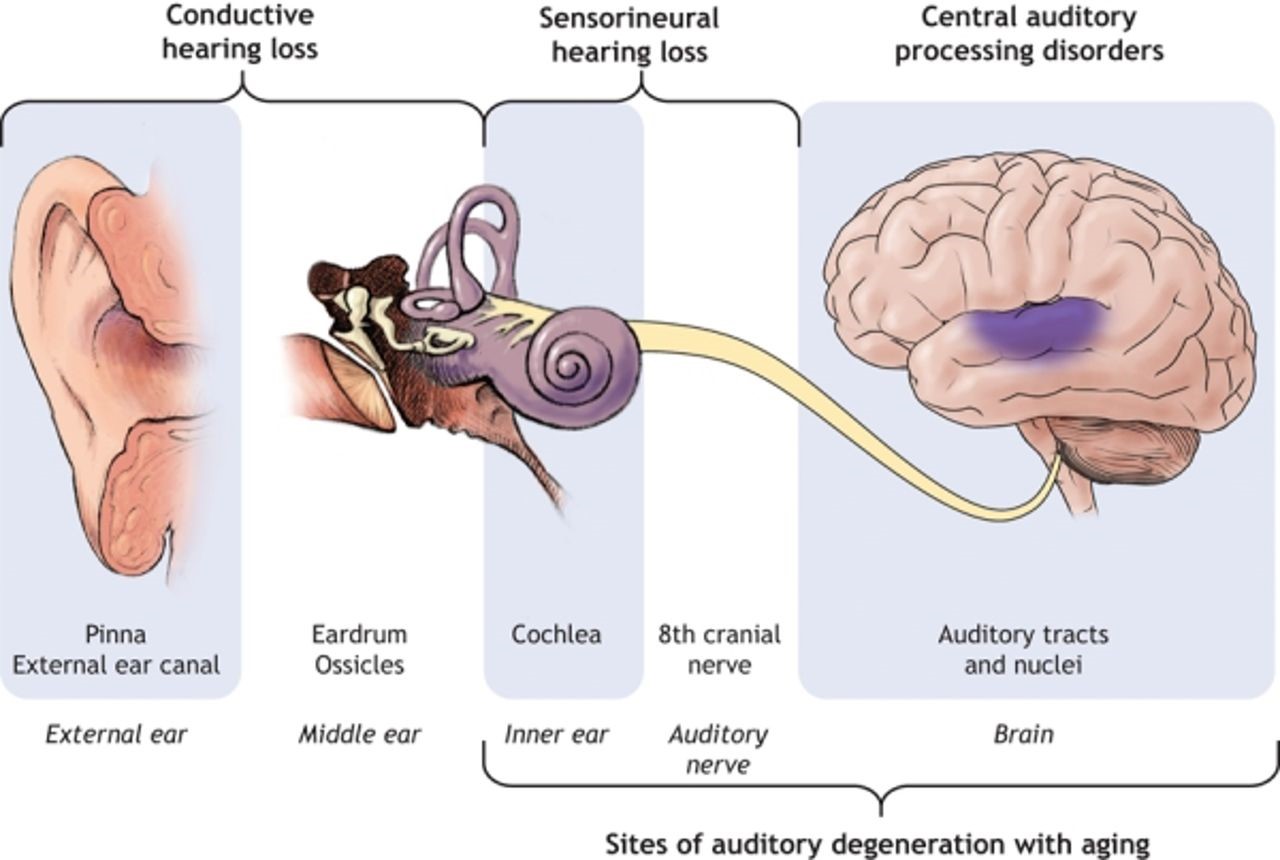
At least 80% of those who are 85 years or older and 50% of adults in their seventh decade suffer hearing loss. Clinicians can address the issue and refer patients to the right specialists by having a thorough understanding of the auditory system and the illnesses that affect each component of it.
Hyperbaric oxygen therapy, vasodilators, and corticosteroids are the three most effective treatments. Only hyperbaric oxygen has undergone enough randomized controlled trials to demonstrate a beneficial therapy impact in meta-analyses of the other options. This exercise outlines the benefits, risks, and protocol for hyperbaric oxygen therapy as a treatment for acute sensorineural hearing loss and emphasizes the importance of the interprofessional team in aiding patients who are seeking treatment as soon as possible [2].
Pathophysiology
The cochlea, a structure in the inner ear that is known to have a high oxygen requirement, maintains hearing function. Progressive ossification, fibrosis, neuronal degeneration, endolymphatic hydrops, and hearing loss are all symptoms of cochlear hypoxia. The organ of the Corti receives little direct blood supply; oxygen must diffuse through the perilymph and cortilymph. The anterior inferior cerebellar artery (85%) or the basilar artery (15%) gives rise to the long, slender labyrinthine artery (internal auditory artery). Through the internal acoustic meatus and into the inner ear, it travels with the vestibulocochlear nerve. Labyrinthine artery closure in animal models has been associated with hearing loss, fibrosis, and gradual degenerative alterations. Hearing loss may develop from any condition that causes arterial blockage of this artery [3].

In the etiological assessment of SNHL, imaging, DNA tests, and screening for congenital infections and metabolic illnesses are frequently carried out. About 50% of all congenital SNHL cases are thought to have genetic causes, of which 70% are thought to be non-syndromic and 30% are syndromic. In 25% of cases of congenital SNHL, an acquired component is discovered. These include risk factors like hypoxia during birth, hyperbilirubinemia, preterm, and a stay in a newborn intensive care unit (NICU) longer than five days, as well as congenital infections (TORCH: toxoplasmosis, others, rubella, cytomegalovirus, and herpes simplex viruses).
Clinical Evaluation
It is crucial to distinguish between conductive and sensorineural hearing loss because, despite similarities in presentation, the two have quite different treatment consequences. Specific questions regarding a history of repeated hearing loss, accompanied tinnitus, vertigo, focal neurological abnormalities, and other symptoms should be asked. During the local ear examination, the tympanic membrane and impacted cerumen are inspected otoscopically for damage (the presence of otitis media with effusion should be specifically looked for). A thorough audiometric test using pure tone and spoken audiometry follows the clinical examination [4].
Laboratory Tests
Complete blood counts, coagulation profiles, serum electrolytes, and erythrocyte sedimentation rates are routine laboratory blood tests that are frequently conducted. According to the clinical practice recommendations of the American Academy of otorhinolaryngology and head and neck surgery (AAO-HNS), the yield is poor and routine blood profiling is not advised. Serological testing for infectious causes ought not to be performed routinely but in response to specific clinical and epidemiological circumstances [5].
Causes
The following factors may contribute to this kind of hearing loss:
- Illnesses
- Hazardous drugs for the hearing
- family history of hearing loss
- Ageing
- an impact on the head
- an issue with the inner ear’s development
Depending on the extent of the damage, SNHL can range from minor hearing loss to total loss of hearing.
- little hearing loss an audible loss of 26 to 40 dB.
- a slight hearing loss. a hearing loss of between 41 and 55 dB.
- profound hearing loss. a hearing loss that is louder than 71 dB.
Symptoms
Following sensorineural hearing loss,
- trouble hearing noises in noisy environments, especially trouble understanding female and child voices
- unsteadiness or balance issues
- difficulty hearing loud noises
- You have the impression that noises and conversations are muffled and that you can hear but not understand them.
- tinnitus (ringing in your ears) (ringing in your ears) [6].
Hyperbaric Oxygen as Effective Medicine for Sensory Hearing Loss
What is HBOT?
By administering pure oxygen under high pressure, hyperbaric oxygen treatment (HBOT) increases the amount of oxygen in the blood and tissues (hyperoxia) (about 2-3 atmospheres). Hyperbaric oxygen therapy, also known as pure oxygen (O2) exposure at high atmospheric pressures, is one type of treatment (HBOT). According to the Undersea and Hyperbaric Medical Society, this pressure may be greater than or equivalent to 1.4 atmospheres (atm) (UHMS). For all current UHMS-approved usage, patients may only use oxygen when restrained in an environment with a minimum air pressure of 2 ATA. A 100% oxygen supply system and pressure chamber—which may be flexible or rigid—are required for hyperbaric oxygen therapy. Trained professionals who monitor the patient and adjust as necessary follow a predetermined plan.
Understanding the high metabolism and lack of vascularity in the cochlea lends support to the justification for using hyperbaric oxygen therapy (HBOT) to treat SSHL. The cochlea and the internal organs need a lot of oxygen. There is not much direct vascular supply, especially to the Corti organ. Through oxygen diffusion from the cochlear capillary networks into the perilymph and the cortilymph, tissue oxygenation of the cochlea’s structures takes place. The main oxygen source for these intracochlear structures is the perilymph. Unfortunately, patients with SSHL have much lower perilymph oxygen tension. The arterial-perilymphatic oxygen concentration differential must be quite large to produce a steady increase in the perilymph’s oxygen content. HBOT can be used to restore this.
In a large number of patients with acute sensorineural hearing loss, hyperbaric oxygen can boost perilymph oxygen tension and restore hearing. The ability to raise oxygen tension in the perilymph and the degree of patency of the labyrinthine artery are two variables that may affect effectiveness. Their advantages over placebo have been demonstrated in numerous prospective randomized controlled trials. Patients who receive treatment within 14 days of the commencement of their symptoms and who also receive concurrent steroids see the highest outcomes (either systemically or intratympanic). If not contraindicated, steroids should be administered at a starting dose of 1 mg/kg/day and reduced over 2 to 3 weeks. Hyperbaric oxygen therapy should be taken into consideration for patients with moderate to severe hearing loss (more than 40 dB). For hyperbaric oxygen therapy, the recommended treatment pressure should be 2.0 ATA to 2.5 ATA for 90 minutes each day for 10 to 20 treatments, depending on response. Less likely to benefit from additional therapy are those who have not improved (10 dB or less) after the first ten sessions [7].
The American Academy of Otolaryngology advises against the routine use of antivirals, thrombolytics, vasodilators, vasoactive drugs, or antioxidants and suggests that hyperbaric oxygen be investigated as a therapy option for up to 3 months following the onset of symptoms. Even ten weeks after the onset of symptoms, patients who have failed an initial course of steroids can frequently still benefit from a combination of intratympanic steroids and hyperbaric oxygen therapy. A comprehensive autoimmune and vasculitis examination, an audiogram, a brain MRI (to rule out retro cochlear pathology), and an auditory brainstem response should all be performed on patients by an otolaryngologist and an audiologist [8].
A 37-year-old Thai guy who had suddenly developed bilateral progressive hearing loss arrived at Burapha University. He was known to have hypertension, which amlodipine effectively managed. He suddenly had tinnitus, auditory fullness, and lost his left hearing. The patient opted to have HBOT (day 36) as a salvage procedure. According to the US Navy treatment table, the HBOT programme was set for 10 sessions (2 ATA 90 minutes). The HBOT was conducted using a 6-seat multi-place chamber, and it began 36 days after the first signs of hearing loss. After the third HBOT treatment (day 38), normal hearing and the absence of tinnitus in both ears were experienced [9].
It is unknown whether adding hyperbaric oxygen therapy (HBOT) to regular medical therapy (MT) can help those with idiopathic SSNHL. In 2401 patients with SSNHL (mean age, 45.4 years; 55.3% female), three randomized clinical trials and 16 nonrandomized studies evaluating outcomes after HBOT + MT vs MT alone were included. The HBOT + MT group significantly outperformed the MT alone group in terms of the pooled odds ratios (ORs) for complete hearing recovery and any hearing recovery (complete hearing recovery OR, 1.61; 95% CI, 1.05-2.44; and any hearing recovery OR, 1.43; 95% CI, 1.20-1.67). Additionally, the HBOT + MT group significantly outperformed the MT alone group in terms of absolute hearing gain. In groups with severe to profound hearing loss at baseline, HBOT as a salvage treatment, and a total HBOT duration of at least 1200 minutes, the benefit of HBOT was larger. Overall hearing improvement was seen in 94% of patients. Within two weeks of the commencement, 82% of patients with severe hearing loss who came to us demonstrated maximum improvement. When compared to other patients, those who received treatment within 14 days experienced the greatest improvement, going from 76 20.06 dB to 51.9 17.1 dB. At frequencies higher than 500 Hz, there was a larger hearing gain. Patients under 50 years old had a gain of 25 13.2 dB, whereas patients over 50 years old had a gain of 19 10.2 dB [10].
The hyperbaric chamber’s pressure must be at least 1.4 ATA for HBOT to be effectively effective in the treatment of SSNHL. The diffusion radius of oxygen from the capillaries to the surrounding tissues increases noticeably only while breathing 100% oxygen at hyperbaric circumstances over 1.4 ATA. Recent studies have shown that increasing the maximum pressure during HBOT above 2.5 ATA has no beneficial effect on hearing recovery; therefore, maintaining an air pressure between 2.0 and 2.5 ATA is currently advised for the treatment of SSNHL [11].
References
- Ahn et al., 2008. J.H. Ahn, M.H. Yoo, T.H. Yoon, J.W. Chung
Can intratympanic dexamethasone added to systemic steroids improve hearing outcome in patients with sudden deafness? The Laryngoscope, 118 (2008), pp. 279-282
https://doi.org/10.1097/MLG.0b013e3181585428
- Battaglia et al., 2008. A. Battaglia, R. Burchette, R. Cueva
Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for the treatment of idiopathic sudden sensorineural hearing loss
Otol. Neurotol., 29 (2008), pp. 453-460
https://doi.org/10.1097/MAO.0b013e318168da7a
- Byl, 1984. F.M. Byl Sudden hearing loss: eight years’ experience and suggested prognostic table. The Laryngoscope, 94 (1984), pp. 647-661 Morton C, Nance W (2006) Newborn hearing screening – a silent revolution. N Engl J Med 354:2151–2164
Link: https://www.nejm.org/doi/full/10.1056/nejmra050700
- Wang Y, Gao Y, Wang B, Chen L, Zhang X. Efficacy and Prognostic Factors of Combined Hyperbaric Oxygen Therapy in Patients with Idiopathic Sudden Sensorineural Hearing Loss. Am J Audiol. 2019 Mar 15;28(1):95-100.
Link: https://pubmed.ncbi.nlm.nih.gov/30938564/
- Lammers MJ, Lea J, Westerberg BD. Extensive Heterogeneity in the Meta-analysis of Hyperbaric Oxygen Therapy for Idiopathic Sudden Sensorineural Hearing Loss. JAMA Otolaryngol Head Neck Surg. 2019 May 01;145(5):483-484.
Link: https://pubmed.ncbi.nlm.nih.gov/30920600/
- Paprocki J, Sutkowy P, Piechocki J, Woźniak A. Markers of Oxidant-Antioxidant Equilibrium in Patients with Sudden Sensorineural Hearing Loss Treated with Hyperbaric Oxygen Therapy. Oxid Med Cell Longev. 2019; 2019:8472346.
Link: https://pubmed.ncbi.nlm.nih.gov/30881599/
- Imsuwansri, Thanarath, Pipat Poonsap, and Kornkiat Snidvongs. “Hyperbaric oxygen therapy for sudden sensorineural hearing loss after failure from oral and intratympanic corticosteroid.” Clinical and Experimental Otorhinolaryngology 5. Suppl 1 (2012): S99-S102.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3369993/
- Rhee, Tae-Min, et al. “Addition of hyperbaric oxygen therapy vs medical therapy alone for idiopathic sudden sensorineural hearing loss: a systematic review and meta-analysis.” JAMA otolaryngology–head & neck surgery 144.12 (2018): 1153-1161.
Link: https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2704029
- Sahni, Tarun, et al. “The role of hyperbaric oxygen therapy in Sudden Sensorineural Hearing Loss: A retrospective review of 50 patients.” Apollo Medicine 11.3 (2014): 208-212.
Link: https://www.sciencedirect.com/science/article/pii/S0976001614000982
- Kujawski, S.; Kujawska, A.; Kozakiewicz, M.; Olszanski, R.; Siermontowski, P.; Zalewski, P. The effect of hyperbaric oxygen therapy on the nervous system. Systematic review. Pol. Hyp. Res. 2015, 4, 19–27.
Link: https://scholar.google.com/scholar_lookup?title=The+effect+of+hyperbaric+oxygen+therapy+on+the+nervous+system.+Systematic+review&author=Kujawski,+S.&author=Kujawska,+A.&author=Kozakiewicz,+M.&author=Olszanski,+R.&author=Siermontowski,+P.&author=Zalewski,+P.&publication_year=2015&journal=Pol.+Hyp.+Res.&volume=4&pages=19%E2%80%9327&doi=10.1515/phr-2015-0020
- Rhee, T.M.; Hwang, D.; Lee, J.S.; Park, J.; Lee, J.M. Addition of hyperbaric oxygen therapy vs medical therapy alone for idiopathic sudden sensorineural hearing loss: A systematic review and meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 1153–1161.
Link: https://jamanetwork.com/journals/jamaotolaryngology/article-abstract/2704029