Role of Hyperbaric Oxygen Therapy in Fibromyalgia
What is Fibromyalgia?
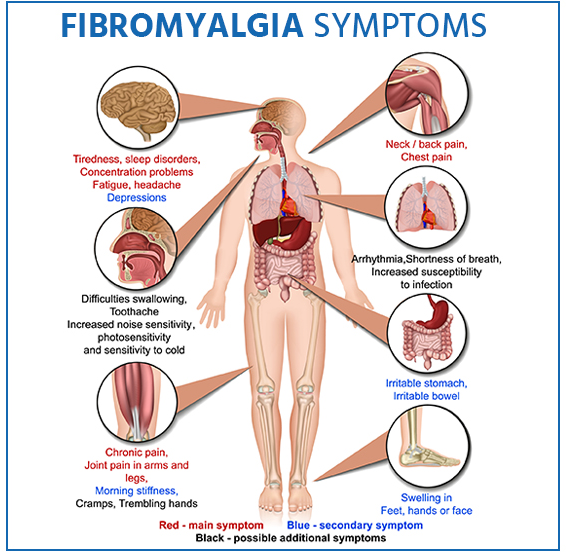
A persistent pain illness called fibromyalgia (FM), or fibromyalgia syndrome (FMS) exists. Widespread or localized pain, stiffness, oedema, and sensitivity in the muscles and joints are some symptoms of FMS. Fatigue, sleep troubles, headaches, anxiety, and memory issues are common symptoms of FMS. Some people also claim to be extremely sensitive to sounds, lighting, odours, and changes in temperature
With a 9:1 female-to-male incidence ratio, fibromyalgia syndrome (FMS) is a chronic and incapacitating condition that affects the quality of life of 2-4% of the population. The central nervous system sensitivity condition known as FMS is a significant typical example that is linked to aberrant brain activity. It is a common cause of persistent widespread musculoskeletal discomfort. In the United States, approximately 5 million persons those are 18 years of age or older have fibromyalgia. According to studies, natal girls are more likely than natal males to suffer from fibromyalgia [1].
Pathophysiology
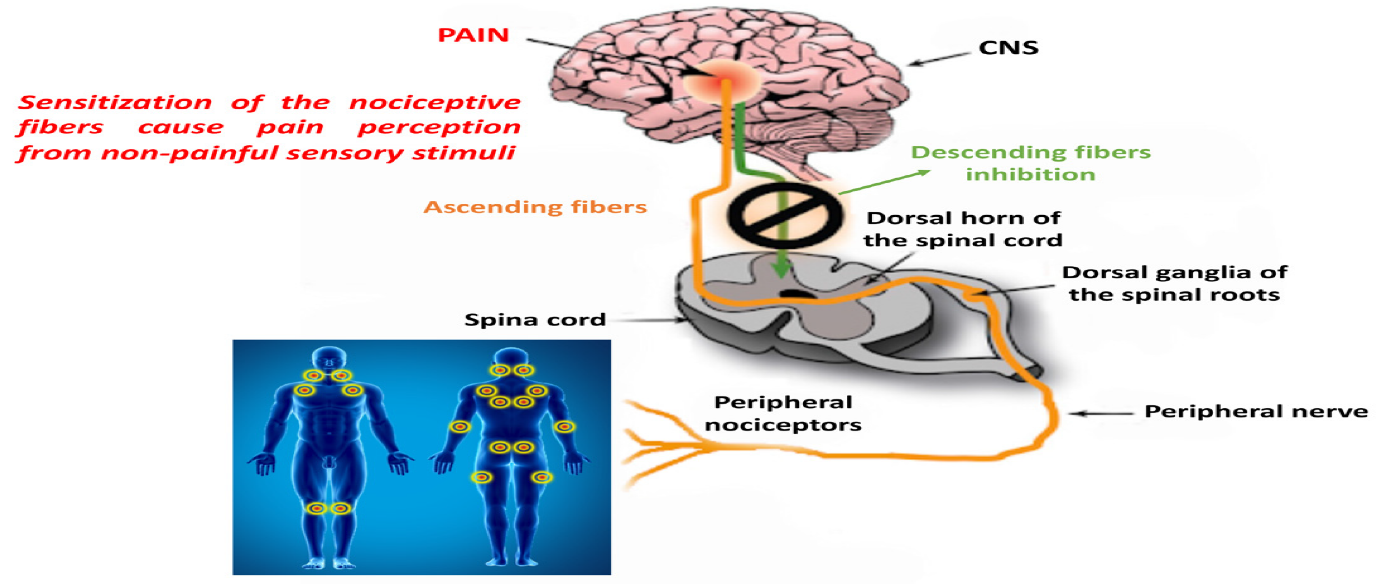
The cause of fibromyalgia is unknown. Researchers have noted imbalances in brain chemicals and growth hormones, as well as abnormalities in central nervous system functions. Substance P, a spinal fluid molecule that amplifies pain signals, maybe three times more concentrated in fibromyalgia patients than it is in healthy individuals. Many people blame a specific incident, ailment, or traumatic experience for the development of fibromyalgia. The illness does not worsen and does not harm tissues, joints, or bones.
Pain processing disorders include fibromyalgia. Evidence suggests that the central amplification of pain signals is caused by aberrant functioning of the ascending and descending pain pathways, which is comparable to turning up the “volume control setting” on a stereo. The levels of several neurotransmitters known to facilitate pain transmission are elevated in the cerebrospinal fluid and brain, and levels of several neurotransmitters known to inhibit pain transmission are decreased in FM patients. These changes in neurotransmitter levels result in enhanced central nervous system pain processing [2].
Changes in Brain in FMS
The processing of the information by the brain and the relevant sensors at the site of the pain determines the intensity of the pain feeling. Somatosensory cortex activity was increased in FMS patients compared to healthy controls, but frontal, cingulate, medial temporal, and cerebellar cortex activity was decreased. Other fMRI research discovered that depressive symptoms were connected to the pain response in regions of the brain that are involved in assigning and interpreting the pain feeling, but not in regions that receive sensory information [3].
Symptoms
The most typical fibromyalgia signs and symptoms are as follows:
- There is a great deal of pain; fibromyalgia pain is typically described as a chronic
- Fatigue
- Cognitive issues [4].
Fibromyalgia frequently co-occurs with other conditions, including:
- Rheumatoid bowel syndrome (IBS)
- Irritable Bowel Syndrome (CFS)
- headaches of all kinds, including migraines
- A condition when the bladder is inflamed is interstitial-cystitis, also referred to as painful bladder syndrome.
- Temporomandibular joint disorders
- Anxiety
- Depression
- Postural tachycardia syndrome
Risks and causes
When the reaction of the brain and spinal cords changes because of repeated nerve stimulation, fibromyalgia symptoms become apparent. This change is brought on by an aberrant increase in the brain’s concentration of chemicals that signal pain. Additionally, pain receptors in the brain develop a form of pain memory and become sensitized, which could cause them to respond to both painful and nonpainful signals.
1. Genetics – Because fibromyalgia is a hereditary condition, having certain genetic changes may increase your risk of developing it.
2. Infections – Some illnesses seem to cause or make fibromyalgia worse
3. Tragedies, either physical or psychological – Fibromyalgia can occasionally be brought on by a physical incident, such as a car accident. The onset of the illness may also be influenced by long-term psychological stress [5].
Hyperbaric Oxygen as Effective Medicine for Fibromyalgia
How does it work?
Hyperbaric oxygen therapy, also known as HBOT, is a treatment that increases the amount of oxygen in blood and tissues by delivering pure oxygen at high pressure. The pressure may be greater than or equal to 1.4 atmospheres (atm). This pressure may only be kept for up to 10 minutes at a time so that patients may not get any negative effects from breathing pure oxygen for too long.
How HBOT treats Fibromyalgia?
It has been demonstrated that hyperbaric oxygen therapy (HBOT) lessens the discomfort brought on by fibromyalgia and other chronic pain illnesses. Some researchers think HBOT also alters brain activity related to disorders that cause chronic pain.
A clinical trial of 60 FMS Patients treated with HBOT
In a clinical trial, patients were randomly assigned to crossover and treatment groups, and those in the treated group underwent baseline and HBOT evaluations. Three evaluations were conducted on patients in the crossover-control group: at baseline, following a control period during which no therapy was given, and after HBOT. Physical examinations, which included measuring the number of tender points and the pain threshold, detailed assessments of the quality of life, and single photon emission computed tomography (SPECT) imaging tests to measure brain activity were all included in the evaluations. The HBOT treatment included 90 minutes of 100% oxygen, spread across 40 sessions, five days a week, at 2ATA. 60 female patients with FMS who were at least two years older in diagnosis and ranged in age from 21 to 67 were included. With a considerable increase in life quality, HBOT significantly reduced all FMS symptoms in both groups. Analysis of the SPECT images showed that the abnormal brain activity had been corrected, with the hyperactivity decreasing mostly in the posterior region and the lowered activity increasing primarily in the frontal regions. After the control period, no improvement in any of the metrics was seen. The study offers proof that HBOT can help FMS patients with their symptoms and quality of life. Additionally, it demonstrates how HBOT can promote neuroplasticity and significantly correct aberrant brain activity in regions associated with pain in FMS patients [6].
A clinical trial of 50 FMS patients
50 FM patients participated in a randomized clinical study: 26 completed fifteen 90-minute HBOT sessions at 2.4 ATA over three weeks, and 24 received a sham therapy of fifteen 90-minute air-breathing sessions at 1 ATA. Before the first HBOT or sham session, as well as after the fifteenth, they counted the tender sites, algometer pain thresholds, and VAS pain scores. As early as the first HBOT session and continuing through the fifteenth, there was a substantial reduction in the number of tender spots and pain thresholds in the HBOT group compared to the sham treatment group [7].
A randomized controlled experiment including 49 female FMS patients was conducted. This group’s participants had low-pressure hyperbaric oxygen therapy, which included 40 sessions totalling 90 minutes and five sessions each week. 100% oxygen with air pauses at 1.45 ATA was utilized to prevent anxiety and irritability32. The participants in the hyperbaric chamber received oxygen that was purified to 97% using a mask. This group’s members participated in the following protocol-based low-intensity physical exercise program: There are a total of 16 sessions, two of which last 60 minutes. The findings imply that low-pressure hyperbaric oxygen therapy and an eight-week low-impact exercise programme both enhance some muscles’ pain pressure thresholds at rest, endurance, and functional capacity as measured by the distance walked, as well as physical performance in daily tasks. Only low-pressure hyperbaric treatment effectively reduced rest-induced weariness and pain perception. Therefore, low-pressure hyperbaric oxygen therapy may be the preferred course of treatment for FM patients who report severe discomfort and exhaustion [8].
In this study, 33 female FM patients between the ages of 29 and 63 were enrolled. Patients were registered at the Rheumatology Unit San Cesario-Italy after receiving initial pharmacological treatment (Pregabalin 150 mg/diet, Duloxetine 60 mg/diet) with unsatisfactory clinical improvement. The HBOT protocol had 20 treatments, three days a week, 90 minutes, and 100% oxygen at 2.5ATA. Patients were randomly assigned to treated or control groups, and they underwent monthly evaluations for the following four months. Patients in group A received 20 sessions of HOBT treatment in the first two months, and they were assessed for the following two months; patients in group B received pharmacological treatment for the first two months, and then they received 20 sessions of HOBT treatment in the final two months. No pharmaceutical therapy was permitted during HOBT. With a significant increase in life quality, HBOT significantly reduced all FM symptoms. The number of tender points in the two groups decreases because of HOBT. The subsequent two months of observation show no change in this reduction in group A. The improvement in group B is more intricately linked to the HOBT than to the therapy. Group A sees an increase in the FIQ score. There was no improvement seen in the control group [9].
A total of twenty 90-minute sessions of HBOT (100 percent oxygen at 2.5 atm) were performed on patients with FM in different research. Before and following ten and twenty sessions, patients’ health-related quality of life, pain, exhaustion, sleep quality, anxiety and depressive symptomatology were all prospectively evaluated. Of the 32 trial participants, 28 finished all 20 HBOT sessions. After 10 and 20 sessions, pain scores and anxiety and depressive symptom ratings (although not exhaustion) improved, whereas fatigue and the intensity of FM symptoms improved only after 20 sessions. The level of sleep did not significantly change. The negative consequences were minimal [10].
References
1. Clauw DJ, Arnold LM, McCarberg BH. The science of fibromyalgia. Mayo Clin Proc. 2011; 86(9): 907–11. 10.4065/mcp.2011.0206
Link: https://www.sciencedirect.com/science/article/abs/pii/S0025619611652233
2. Arnold LM, Crofford LJ, Mease PJ, Burgess SM, Palmer SC, Abetz L, et al. Patient perspectives on the impact of fibromyalgia. Patient Educ Couns. 2008; 73(1): 114–20. 10.1016/j.pec.2008.06.005
Link: https://www.sciencedirect.com/science/article/pii/S0738399108002796
3. Uceyler N, Zeller D, Kahn AK, Kewenig S, Kittel-Schneider S, Schmid A, et al. small fiber pathology in patients with fibromyalgia syndrome. Brain. 2013; 136(Pt 6): 1857–67.
Link: https://academic.oup.com/brain/article/136/6/1857/618249
4. Harris, R.E.; Clauw, D.J. Imaging central neurochemical alterations in chronic pain with proton magnetic resonance spectroscopy. Neurosci. Lett. 2012, 520, 192–196.
Link: https://www.sciencedirect.com/science/article/pii/S0304394012004120
5. O’Brien, A.T.; Deitos, A.; Trinanes Pego, Y.; Fregni, F.; Carrillo-de-la-Pena, M.T. Defective Endogenous Pain Modulation in Fibromyalgia: A Meta-Analysis of Temporal Summation and Conditioned Pain Modulation Paradigms. J. Pain 2018, 19, 819–836
Link: https://www.sciencedirect.com/science/article/abs/pii/S1526590018300737
6. Efrati S, Golan H, Bechor Y, Faran Y, Daphna-Tekoah S, Sekler G, Fishlev G, Ablin JN, Bergan J, Volkov O, Friedman M, Ben-Jacob E, Buskila D. Hyperbaric oxygen therapy can diminish fibromyalgia syndrome–prospective clinical trial. PLoS One. 2015 May 26;10(5): e0127012. doi: 10.1371/journal.pone.0127012. PMID: 26010952; PMCID: PMC4444341.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4444341/
7. YILDIZ S, KIRALP MZ, AKIN A et al.: A new treatment modality for fibromyalgia syndrome: hyperbaric oxygen therapy. J Int Med Res 2004; 32: 263-7.
Link: https://journals.sagepub.com/doi/abs/10.1177/147323000403200305
8. Izquierdo-Alventosa R, Inglés M, Cortés-Amador S, et al. Comparative study of the effectiveness of a low-pressure hyperbaric oxygen treatment and physical exercise in women with fibromyalgia: randomized clinical trial. Therapeutic Advances in Musculoskeletal Disease. 2020;12. doi:10.1177/1759720X20930493
Link: https://journals.sagepub.com/doi/10.1177/1759720X20930493
9. Muratore, M., et al. “THU0512 Hyperbaric oxygen therapy (HBOT) treatment in fibromyalgia.” (2018): 461-461.
Link: https://ard.bmj.com/content/77/Suppl_2/461.3
10. Atzeni F, Casale R, Alciati A, Masala IF, Batticciotto A, Talotta R, Gerardi MC, Salaffi F, Sarzi-Puttini P. Hyperbaric oxygen treatment of fibromyalgia: a prospective observational clinical study. Clin Exp Rheumatol. 2019 Jan-Feb;37 Suppl 116(1):63-69. Epub 2019 Feb 6. PMID: 30747099.
Link: https://pubmed.ncbi.nlm.nih.gov/30747099/

